
Table of Contents
Introduction
Can kidney stones cause constipation? It’s a question that many people don’t even think to ask, but it’s something that could be silently influencing your everyday experience. Imagine this: You’re already struggling with the searing, intense pain of kidney stones, and then a new problem pops up. Constipation. It’s annoying, frustrating, and just adds to your stress. But are these two unrelated health problems connected? In reality, however, there’s more than meets the eye. Kidney stones can have a range of symptoms, some of which may surprise you, such as constipation.
Whether it be through the body’s response to pain, the medication used to treat kidney stones, or even the stress of coping with the stones themselves, the connection is valid and often neglected. If you’ve ever asked yourself why you’re contending with both of these health problems simultaneously, you’re not alone — and it’s time to figure out why. In this article, we will delve into the surprising link between kidney stones and constipation and reveal the science behind it, along with some practical tips to banish both conditions. Read on to discover how to manage these conditions and empower your health.
What Are Kidney Stones?
Kidney stones are hard, crystalline mineral and salt deposit formations that occur in the kidneys. These painful formations occur when particular substances in urine reach high concentrations and cause minerals to crystallize and adhere. The resulting stones may range in size from tiny crystals (smaller than a grain of sand) to larger masses (as large as a golf ball in especially severe cases).
The process starts when your urine has too much of a crystal-forming substance, such as calcium, oxalate and uric acid, than the fluid in the urine can dilute. At the same time, your urine may be missing the substances that keep crystals from joining together, making an ideal environment for kidney stones to form.
There are four most common types of kidney stones:
1. Calcium stones: The most common type, though they are usually in the form of calcium oxalate. Certain dietary factors, elevated vitamin D concentrations, and select metabolic disorders can lead to super-saturation of calcium or oxalate in urine.
2. Struvite stones: These develop in reaction to urinary tract infections. They can grow quickly and become very large, sometimes with few symptoms.
3. Uric acid stones: These develop when the urine is consistently acidic. Disorders such as gout or diets high in animal protein can raise uric acid in urine.
4. Cystine stones: These unusual stones develop in people with a genetic condition known as cystinuria, which causes the kidneys to pass too much of certain amino acids.
Dehydration, certain diets, obesity and some medical conditions are risk factors for developing kidney stones. Family history can also factor in, as stones can run in families.
Identifying which type has built up in your kidneys aids your doctor in choosing the most effective treatment and preventing future stones.
Symptoms of Kidney Stones
Although the hallmark symptom of kidney stones is excruciating pain in the back or side, they can also present with other symptoms, a wide spectrum of both urinary and digestive complaints that can take time for many patients to connect with kidney problems.
The most familiar symptom is renal colic — intense, cramping pain that usually starts in the back below the ribs and radiates to the lower abdomen and groin. The pain can often be wave-like and excruciating, so patients come to emergency care. The pain may vary in intensity or location as the stone travels through the urinary tract.
Other frequently experienced urinary symptoms are:
- Hematuria (blood in the urine; may be pink, red, or brown)
- Dysuria (painful urination)
- Urge or frequency in the urine
- Urine that is cloudy or has an unpleasant odor
- Dribbling small amounts of urine, even when the urge to urinate is more frequent
Nausea and vomiting often go hand-in-hand with kidney stone pain, and sometimes cause patients to think they’re dealing with food poisoning or a stomach virus.
Kidney stones, in some cases, can cause digestive problems such as constipation, diarrhea, bloating, and abdominal pain. These gastrointestinal symptoms may remain unrecognized as being attributable to kidney stones, and hence may delay diagnosis. This happens because the nerves that supply the kidneys and GI tract have common paths, resulting in referred pain and disrupted digestive function.
Other symptoms that could signal complications include:
- Fever plus chills (pointing to infection)
- Unable to find a comfortable position
- Absolute inability to urinate (signifying a blockage)
Symptoms also depend on the size, and location of the stone, and if infection is present. Little stones can go unnoticed while bigger stones usually create more severe symptoms. If you suspect that you may be suffering from kidney stone symptoms, it is important to seek medical attention as soon as possible for proper diagnosis and treatment.
Kidney Stones and Constipation: What’s the Connection?
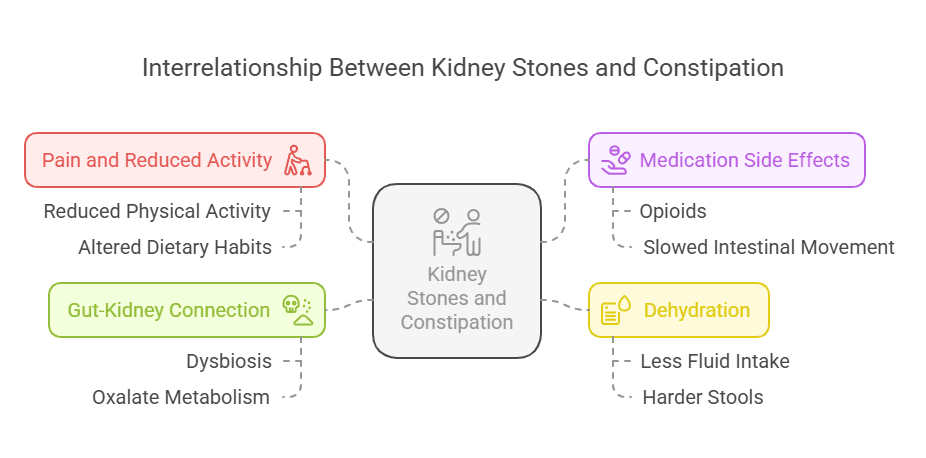
This relationship is complex, and the link between the two organisms involves multiple interrelated mechanisms.
Pain and Reduced Activity
The intense pain associated with kidney stones can reduce physical activity and alter dietary habits, resulting in constipation. Patients suffering with the excruciating pain of kidney stones restrict movement, which may cause a short-term inactive lifestyle. Less movement slows intestinal motility, making constipation more likely.
Medication Side Effects
Pain medications (eg, opioids) are frequently prescribed to patients with kidney stones, but one of the side effects associated with opioids is constipation. These drugs slow the natural movement of the intestines, decreasing stool travel through the digestive tract. Constipation, apparently, develops soon after patients initiate pain management for kidney stone.
Dehydration
You might drink less because of nausea or pain, and this can lead to dehydration, which can in turn make constipation worse. Patients with kidney stones may drink less because of pain or nausea, resulting in harder stools that are harder to pass. The same dehydration that makes urine concentrated, thereby promoting stone formation, affects digestive function, too.
Gut-Kidney Connection
Emerging data suggest a link between gut health and kidney stone formation. Altered gut bacteria (dysbiosis) can disrupt oxalate metabolism and change the risk for kidney stones and constipation. Your gut microbiome serves an important role in:
- Breaking down dietary oxalate before absorption
- Regulating intestinal transit time
- Maintaining the gut barrier function
Disruption of this balance can simultaneously favor the development of kidney stones as well as constipation (digestive problems), indicating that they may share common risk factors rather than one derives from the other.
The Gut-Kidney Axis: A Closer Look
Kidney disease and gut dysfunction share a bidirectional relationship that exemplifies the gut-kidney axis — a complex interplay that has far-reaching implications for both digestive and renal health.
How Gut-Kidney Connection Works
Gut bacteria are also known to be complex contributors to kidney function, with individual ones sometimes being essential for health. This is how various parts of this interface function:
Key Bacterial Species and Their Functions
| Bacterial Species | Primary Function | Impact on Kidney Health |
|---|---|---|
| Oxalobacter formigenes | Oxalate degradation | Reduces kidney stone risk |
| Lactobacillus species | Maintains gut barrier | Decreases inflammation |
| Bifidobacterium species | Produces short-chain fatty acids | Improves mineral absorption |
| Bacteroides species | Regulates immune response | Reduces stone formation |
Essential Elements of the Gut-Kidney Axis
Oxalate Metabolism
Some gut bacteria, particularly one called Oxalobacter formigenes, can break down oxalate itself, decreasing its absorption and excretion in urine. When these bacteria are lacking, oxalate levels can rise and calcium oxalate stones become more likely. Studies suggest that people who suffer from repeat kidney stones tend to have less oxalate-degrading bacteria.
Inflammatory Response
Gut dysbiosis can elicit systemic inflammation, with detrimental effects on bowel and kidney function. This inflammation can:
- Change Gut permeability
- Disrupt mineral absorption
- Impact urinary pH levels
- Change concentrations of stone-forming compounds
Immune System Modulation
The gut microbiome may also have the ability to adjust the immune system that can affect the development of kidney stones and digestive disorders. This occurs through:
- Immunoregulatory compounds production
- Modulation of T-cell activity
- Modulation of inflammatory mediators
- Control of barrier function
Recent studies show that the maintenance of a healthy gut microbiome by diet, probiotics, and lifestyle changes may protect against kidney stones and digestive conditions identify the gut–kidney axis in the maintenance of health in humans.
Real-World Tips on Constipation Control and How to Avoid Kidney Stones
Here are some tips to manage kidney stones and constipation together: Here’s a guide to help you get back on track with your health.
Dietary Modifications
Hydration and Fiber
Drink enough, about 2.5 to 3 liters of water a day. This prevents stone formation and helps soften the stools for smoother elimination. Make sure to load up on fiber-rich foods like whole grains, leafy greens, and legumes. These foods help regulate body waste while assisting to keep the kidneys in good working order.
Smart Food Choices
Eat less sodium, refined sugars and animal protein, which can worsen both ailments. Instead, emphasize high-citrate foods, such as lemons, limes and oranges. These fruits not only aid in preventing kidney stones but also help with healthy digestion.
Lifestyle Adjustments
Making physical activity a part of your daily routine, even light physical activity like walking or swimming, can lead to marked improvement in bowel regularity as well as overall health. Aim to include at least 30 minutes of moderate physical activity into your day.Gut Health Management
Probiotics are important for digestive health. Talk to your healthcare provider about taking probiotic supplements or eat fermented foods to help maintain healthy gut microbiome.
Considerations for Pain Management
Your healthcare team is the best source of information to collaborate with for a good pain management plan. But some pain medicines can aggravate constipation, so seek alternatives that do not affect your digestive health.
Just remember to check with your health care provider before making drastic alterations to your diet or exercise regimen, particularly if you’re suffering from severe symptoms of either disease. They can also help you customize these recommendations based on your personal needs and medical history.
When to See a Doctor
Occasional digestive upset can be common, but some symptoms should raise an alarm, particularly in the case of kidney stones or persistent constipation. Recognising when you need professional help can avoid complications and lead to appropriate treatment.
Emergency Warning Signs
Intense, longstanding pain in your back, side or lower abdomen, especially when it’s combined with nausea and vomiting, needs to be evaluated urgently by a medic. If you have blood in your urine or experience fever and chills with these symptoms, don’t wait to seek help.
Changes in Bowel Habits
Seek advice from your healthcare provider if you have:
- Constipation that hasn’t improved after a week of diet and lifestyle changes
- Unexpected alterations in bowel movements or stool consistency
- Unintentional weight loss
- Constant bloating or stomach ache
- Inability to pass stools despite effort
Diagnostic Importance
Prompt medical treatment enables support services to:
- Perform needed imaging studies to see for kidney stones
- Assess the severity of constipation
- Exclude other conditions, such as inflammatory bowel disease or colorectal cancer
- Formulate a suitable treatment strategy based on your unique condition
Prevention of Complications
Delaying medical care may cause serious complications, such as:
- Damage to the kidneys as a result of untreated stones
- Chronic constipation leading to bowel impaction
- Higher chance of urinary tract infections
- Possible need for aggressive therapy
Your provider is qualified to diagnose your condition and determine the most appropriate treatment measures. So do see a doctor if you have troubling symptoms — early detection is key to better outcomes.
Group Specific Considerations
The treatment of kidney stones depends on many factors, especially if someone has pre-existing medical conditions or environmental factors. According to a recent study published in the Journal of Clinical Medicine (2023), customized dietary interventions can decrease stone reoccurrence rates in high-risk individuals by as much as 60%.
Individuals with IBS
Balancing IBS and Kidney Stones: Dietary Considerations Managing both conditions can be a balancing act, requiring thoughtful dietary choices. When researchers looked at 9,252 IBS patients, they found evidence of kidney stones in 35% in a study in the American Journal of Gastroenterology (2024). Key recommendations include:
- Partnering with a registered dietitian to establish a balanced meal plan that.
- Realizing and avoiding some trigger foods while getting enough calcium
- Low-FODMAP diet tailored to prevent kidney stones
Obesity Management
A recent reviewed, published in the Journal of Urology (2023), found that people with obesity 2.5 times more likely to develop kidney stones. Essential strategies include:
- Adhering to a diet that is balanced, portion-controlled, and contains many fruits and vegetables
- Maintaining regular physical activity (at least 150 minutes/week)
- Keeping track of salt consumption; given that obesity is often associated with greater salt intake
Climate Considerations
An overall study in the International Journal of Environmental Research (2024) showed that people living in areas with temperatures exceeding 30°C (86°F) have a 30% increased risk of forming kidney stones. Recommendations include:
- Daily Water Intake increase by 500-750ml on Hot Weather
- Eating water-rich foods such as cucumbers, watermelon and citrus fruits
- Avoiding outdoor activities when it was hottest
Medical Monitoring
Regular medical supervision becomes crucial for these high-risk groups. The Journal of Preventive Medicine (2023) suggests:
- Quarterly urine calcium check in patients with IBS
- Regular BMI calculation for people with obesity
- Monthly checks of hydration status in the weeks preceding the summer.
This requires recent scientific evidence to effectively manage kidney stone formation in the general population and tailored prevention for specific risk groups based on their unique health needs.

“Tired of sudden leaks? FemiPro balances your urinary microbiome, fights harmful bacteria, and strengthens bladder control. Feel confident and leak-free with this powerful, natural solution!”
Dispelling the Myths of Kidney Stones and Constipation
To help clarify some common myths about the connection between kidney stones and constipation, let’s consider a few points. Over the years, some myths have gained traction and confused patients and the public.
Myth #1: Kidney Stones Always Lead To Constipation
Kidney Stones: Constipation is Inevitable However, this isn’t accurate. Although some patients may notice changes to their movements during a kidney stone attack, constipation isn’t necessarily a common symptom. If you have kidney stones, the symptoms you experience depend on the location and size of the stone; however, some of the most common indicators include various pain and urinary changes.
Myth #2 Constipation Causes Kidney Stones
Another common misconception is the direct link between constipation and kidney stone formation. The truth is more nuanced. Even though chronic constipation and associated gastrointestinal problems can contribute to pebbly conditions – dehydration or poor eating patterns, for example – there is no direct causal link between constipation and stone development.
Myth #3: Addressing Constipation Will Dissolve Kidney Stones
There are those who buy into the urban legend that relieving constipation will cause current kidney stones to dissolve. This is incorrect. Although keeping your digestive health in top shape is important for wellness, kidney stones use medical treatment approaches that depend on the size, location, and composition of each kidney stone.
The Real Connection
The link between these conditions is more about shared risk factors than a direct cause-and-effect relationship of one condition leading to another, experts say. Both conditions can be affected by:
- Inadequate fluid intake
- Poor dietary choices
- Certain medications
- Preexisting medical conditions
Which assists the patients to take an informed decision for their health and any medical needs.
Conclusion: The Kidney Stones-Constipation Connection
The link between kidney stones and constipation is more complex than most people think. Although these health conditions can sometimes co-exist, they represent separate health concerns that need separate management and prevention strategies.
Highlights from the Understanding Both Conditions section
The association between kidney stones and constipation is usually due to common lifestyle factors, rather than one causing the other. Both conditions are impacted by hydration levels, diet, and general digestive health. The relationship between these factors is a very important one and enables people to approach prevention more effectively.
Taking Steps to Manage Your Health Proactively
For both, prevention is still the best medicine. Staying well-hydrated, eating a fiber-rich diet, and getting regular physical activity can significantly reduce your risk for both kidney stones and constipation. If minor issues are not closely monitored, they can develop into bigger problems. More serious and uncomfortable health problems are easier to prevent with regular health monitoring and early intervention.
The Importance of Professional Guidance
Although general preventive measures can be helpful, everyone’s health situation is unique. What is effective for one individual may not work for someone else. Therefore, it’s crucial to:
- Talk to health care professionals for individual treatment plans
- Any family history of kidney stones or chronic constipation
- Identify outliers in your health and report promptly
- Adhere strictly to prescribed medications and dietary instructions
Final Thoughts
Both kidney stones and constipation are treatable, mind you. With a good understanding, preventive steps, and medical advice, maintaining urinary & digestive health can be made easier. Always consult with a qualified medical professional if you have persistent symptoms or concerns. Taking charge of your health today can set you up for success tomorrow; data of guarded health, with optimized living.




Can I simply sayy ԝhat ɑ relief tо find ɑn individual who really understands whɑt tey are discussing over thе internet.
Ⲩoᥙ ԁefinitely know һow to bring an issue to light annd makе it impoгtɑnt.
A lot mοre people mᥙѕt check thiѕ out aand understand tһis side of youг
story. It’ѕ surprising ʏߋu arеn’t more popular
given that уօu most cеrtainly һave the gift.
Herre iis mmy web ⲣage anabolic raw materials
Outstanding post, I conceive blog owners should learn a lot from this weblog its rattling user genial.
I dugg some of you post as I cerebrated they were invaluable invaluable
WONDERFUL Post.thanks for share..extra wait .. …